IRON MOUNTAIN, Mich. (WZMQ) – The Oscar G. Johnson VA Medical Center (OGJVAMC) reallocated staff from its inpatient acute care unit to address a nearly 20% increase in the Community Living Center’s daily census starting this June. This shift came as part of a broader effort to manage resources efficiently amid a projected $4.5 billion National VA budget deficit, while still expanding and optimizing care for veterans.
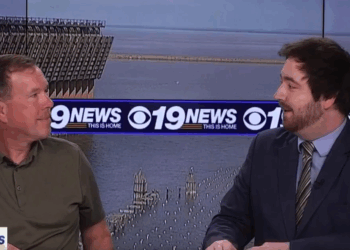
Chris Mapps, President of the American Federation of Government Employees Local 2280, voiced concerns over the reassignments and thinks the appropriations and extra authorities given to the VA through the PACT act were mismanaged. “The staff are getting reassigned. They shut down acuity so that they can specifically reassign them, because we don’t have enough staff to cover everything,” he said. Mapps highlighted the challenges faced by the nursing staff, particularly due to the nationwide hiring freeze, which he says has exacerbated existing staffing issues. He cited that the changes have led to concerns about only 1 RN per night shift in acute care.“The consequences were immediate because we already had staffing issues in nursing.”
The acute care unit averages about 4 patients a day, currenty. Dr. John P. Shealey, the Director of OGJVAMC, assured that patient safety remains the top priority, and assured that the hospital is appropriately staffed. “We do have adequate staffing to meet our needs here for all of our patients. We maintain the appropriate staffing ratios for that,” stated Dr. Shealey, adding “Because we also have an onsite nursing home, they have 24/7 care there as well, and so we have a multitude of nurses and aids and LPN’s and so on as part of the care team there as well. So, because we’re one entity, we’re able to cross-cover as-needed.” A typical nursing ratio is about 4-5 patients per RN.
Dr. Shealey also detailed the measures in place to ensure continued care quality. “We utilize LPNs, CNAs, and other members of the care team to support our RNs, ensuring no nurse is left alone during night shifts,” he explained. “We do have surge plans in place… to get us through any pandemic, natural disaster, or even a surge in needing to take care of patients here.”
Mapps, however, expressed concerns about the long-term implications of the staffing, despite zero jobs being cut with the transition of staff from acute care to nursing home care. “We don’t have all the information on what’s going to happen… If we don’t start hiring soon, it’s going to lead to not enough staff and burnt-out staff that leads to safety concerns for staff and patients.”
Despite the national budget constraints, OGJVAMC has managed to expand its services, with plans to introduce a pain specialist and potentially rheumatology and dermatology in the near future. Dr. Shealey emphasized the center’s commitment to growth. “We’re still in a growth mindset… We’ve added gynecology for women’s healthcare, a gastrointestinal provider, and neurology,” he said. “We will be adding a pain specialist very soon.”
Dr. Shealey also highlighted the impact of the PACT Act, which significantly broadened eligibility for VA benefits, leading to record hiring in 2023 and the enrollment of 800 veterans into care at OGJVAMC. “The PACT ACT significantly broadened eligibility for VA benefits and expanded eligibility for healthcare to more veterans than ever before,” he noted.
The facility’s director reassured that strategic adjustments were being made to balance resources effectively. “It’s a delicate balance… We adjust our hiring strategically according to patient needs,” Dr. Shealey stated. He also confirmed that communication had been extensive with both staff and local facilities to ensure everyone was informed of the changes.
As OGJVAMC navigates these financial and staffing changes, the administration remains hopeful for relief with the new federal budget in October. “My hope is that this all will end in October when we get the new federal budget,” Dr. Shealey said. Meanwhile, the center continues to prioritize key areas such as suicide prevention, mental health, and women’s healthcare, in line with directives from the VA Secretary.